The National Health Service is a beloved British institution, providing care for millions based on need, not the ability to pay. However, with an ever-growing and ageing population, the financial pressures on the service are a constant source of debate. To understand the challenges it faces, we must look beyond the headline budget and examine where the money comes from, and where it is lost through fraud, systemic waste, and the complex demands of 21st-century Britain.
It is interesting to note that when Labour came into power in 2024, they announced an additional £22.6 billion in resource spending for the NHS in England for the current year and the next, which was described as the largest increase in the health service's funding since the pandemic.
However, it appears that this money has simply been 'swallowed up' without any real improvement in services.
The Staggering Cost of Funding the NHS
The National Health Service is funded primarily through general taxation, with a smaller portion coming from National Insurance contributions. Its budget is one of the largest of any public service in the UK.
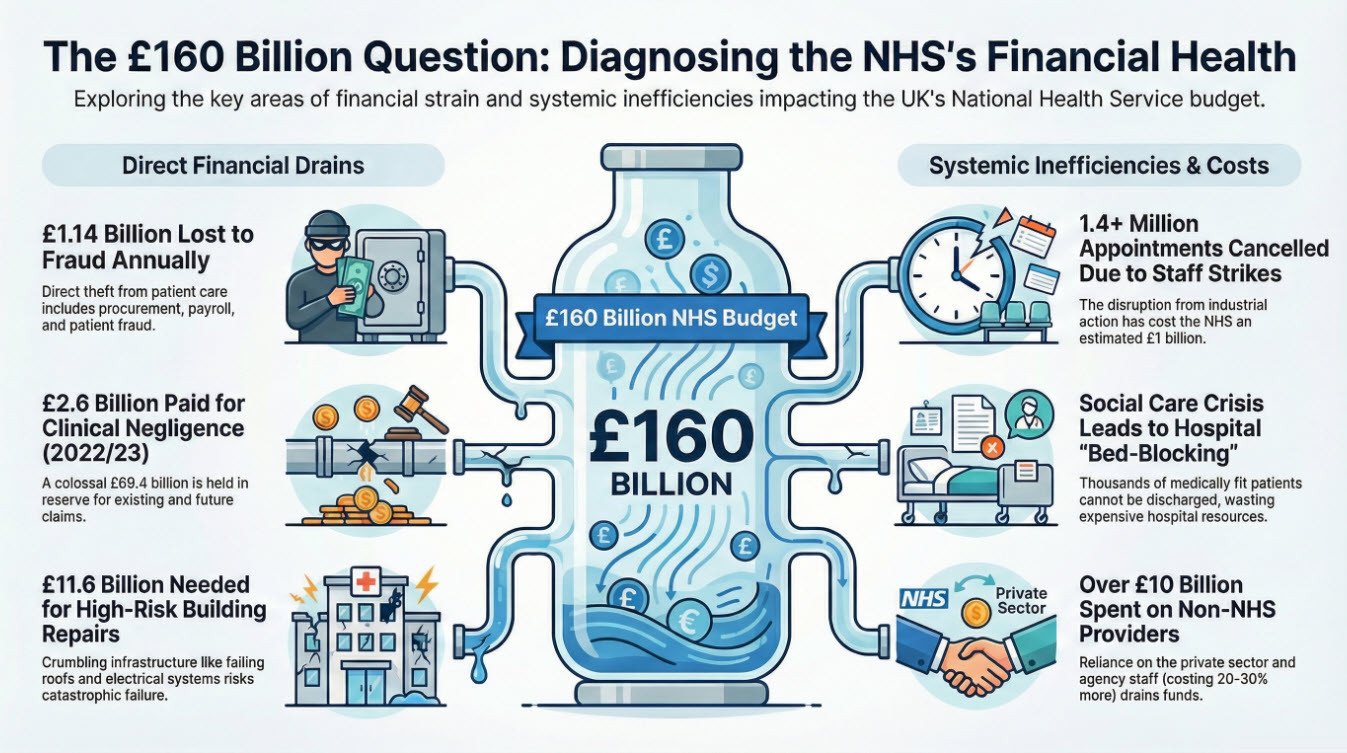
For the 2023/24 financial year, the Department of Health and Social Care (DHSC) budget was over £160 billion. This figure has risen significantly due to the COVID-19 pandemic backlog and government funding pledges.
- Source: The Institute for Fiscal Studies (IFS) notes that health spending has grown as a share of national income, reflecting political choices and the rising cost of healthcare technologies and an ageing population.
- Context: A significant portion of every pound paid in tax goes directly towards funding the health service, raising critical questions about value for money and long-term sustainability.
The Hidden Drain: Fraud and Theft in the NHS
While the vast majority of staff are dedicated and honest, the scale of fraud against the service is substantial and represents a direct theft from patient care.
The NHS Counter Fraud Authority (NHSCFA) estimates that fraud costs the National Health Service an estimated £1.14 billion per year. This is not petty theft; it is a sophisticated and persistent problem encompassing procurement, payroll, and patient fraud, apart from the theft of medical supplies.
- Source: The NHS Counter Fraud Authority (NHSCFA) details these figures in their annual "Fraud, Bribery and Corruption Report."
Where is Money Being Wasted? The Systemic Challenges
Beyond criminal fraud, there are deep-rooted inefficiencies that drain vital resources. Identifying these is key to building a more resilient National Health Service.
The Management Conundrum: "Too Many Chiefs?"
A frequent criticism is that the NHS has become top-heavy with managers. While effective management is crucial, there is a perception of a bloated bureaucracy. The number of NHS managers has grown at a faster rate than the number of nurses over the past decade. Critics argue that this expansion creates layers of administration, slows decision-making, and diverts funds from the frontline. The challenge is ensuring that management structures are lean, effective, and support clinical staff, rather than burdening them.
The Social Care Crisis: Blocking Hospital Beds
One of the most costly inefficiencies is the lack of ongoing social care. Thousands of patients who are medically fit for discharge remain in hospital beds because there is no suitable care package available for them at home or in a residential facility. This phenomenon, known as "bed-blocking," has a double cost: it wastes expensive acute hospital resources and leaves patients in an inappropriate environment.
This crisis was exacerbated by the mandatory vaccination policy for care home staff during the COVID-19 pandemic. While intended to protect vulnerable residents, the policy led to the dismissal of an estimated 40,000 care workers (Source: Skills for Care). This sudden exodus severely damaged an already fragile workforce, further reducing care capacity and intensifying the pressure on NHS beds.
The Sky-High Cost of Temporary Staff
Driven by workforce shortages, the NHS spends billions on temporary agency staff. NHS Providers highlights that trusts can pay up to 20-30% more for an agency doctor or nurse compared to a permanent member of staff. This is a direct result of failing to train and retain enough permanent staff.
Paradoxically, there are reports of British-trained medical staff struggling to secure specialist training posts (FY3/FY4) due to intense competition, leading to a "brain drain" as they seek opportunities abroad. This points to a critical failure in workforce planning, where the NHS both relies on expensive temps and fails to fully utilise its own homegrown talent.
The Real-World Costs of a Diverse Population
Mass immigration brings immense cultural and economic benefits to the UK, but it also presents specific, tangible costs to the NHS that are rarely discussed.
- Translation Services: Providing professional interpreters for hundreds of languages is a non-negotiable for patient safety and equitable care, but it comes at a significant cost, running into tens of millions of pounds annually.
- Targeted Healthcare Needs: Some communities have specific health challenges that require dedicated resources. For example, NHS Bradford reportedly spent £40,000 a year on a 'Genetic Risk Equity Midwife' to address the higher incidence of genetic disorders linked to consanguineous (close-relative) marriage. While a vital public health role, this exemplifies how the NHS must adapt and fund services to meet the specific genetic and cultural health needs of its local population, adding another layer of complexity and cost.
The Industrial Action Crisis
One of the most visible and damaging crises in recent years has been the ongoing industrial action by junior doctors and other healthcare staff. These strikes, primarily driven by disputes over pay and working conditions, have had a catastrophic impact on patient care and NHS finances.
The British Medical Association (BMA), the union representing junior doctors, has argued that years of below-inflation pay rises have led to a real-terms pay cut of over 25% since 2008. The resulting strikes have led to:
- Mass Cancellations: Since the industrial action began, over 1.4 million hospital appointments and surgeries have been cancelled or postponed (Source: NHS England).
- A Growing Backlog: Each wave of strikes adds tens of thousands of cases to the already record-high elective care backlog, pushing waiting lists ever closer to 8 million.
- Financial Cost: The strikes have a direct financial impact. The NHS pays a premium to consultants to provide emergency cover during strikes, and the cost of rearranging appointments and managing the disruption is estimated to have exceeded £1 billion.
- Human Cost: Beyond the numbers, the human impact is profound. Patients facing life-altering surgeries, cancer treatments, and vital diagnostics face agonising delays, with their conditions potentially worsening as they wait.
The Private Sector Crutch: Why the NHS is Renting Beds
A clear indicator of the NHS's capacity crisis is its growing reliance on the private sector. NHS trusts don't just "borrow" beds; they pay daily to rent them, along with the surgical teams and equipment that go with them. This is done for several key reasons:
- Clearing the Backlog: The most common reason is to create additional capacity to tackle the enormous waiting lists for elective (planned) care, such as hip replacements and cataract surgeries. By outsourcing thousands of procedures to private hospitals, the NHS aims to prevent waiting lists from growing even longer.
- Shielding from Strikes: During industrial action, the NHS increasingly uses private facilities to protect a small number of critical procedures, particularly cancer surgeries, from cancellation.
- Lack of Physical Space: Many NHS hospitals simply do not have enough operating theatres or recovery beds to run at the required capacity. Renting private space is a short-term fix for this physical constraint.
However, this is a costly solution. While it can be cost-effective for specific procedures, it represents a significant leakage of public funds to private companies. A Nuffield Trust report highlighted that the NHS spent over £10 billion on care from non-NHS providers in a single year, a substantial portion of which goes to private hospitals. This creates a paradox: the NHS is spending vast sums to prop up a private sector that then poaches its staff, rather than investing that money directly into expanding its own permanent capacity.
A Crumbling Foundation: The NHS Estate in Urgent Need of Repair
While staff and funding dominate headlines, the physical state of NHS hospitals and facilities poses a severe risk to patient safety and operational efficiency. A significant portion of the NHS estate is outdated and failing.
The problem is quantified by the NHS Estates Returns Collection, which categorises the risk presented by its buildings. The situation is dire:
- High-Risk Backlog Maintenance: This refers to repairs that are necessary to prevent catastrophic failure, major disruption to clinical services, or safety breaches that could cause harm. The government's own data shows that the cost of this high-risk backlog has risen to an estimated £11.6 billion across England.
- What this looks like in practice:
- Roof Collapses: In 2023, Musgrove Park Hospital in Taunton had to close three operating theatres and a critical ward after a concrete beam holding up the roof was found to be unsafe, leading to massive disruption.
- Failing Infrastructure: At Queen Alexandra Hospital in Portsmouth, corroded steam pipes and electrical systems are so old that engineers struggle to find parts, creating a constant risk of failure that could shut down entire wings.
- Asbestos and Fire Safety: Many older hospitals, like parts of Leeds General Infirmary, are riddled with asbestos. Any renovation work requires incredibly expensive and slow remediation, and the buildings often do not meet modern fire safety standards.
The financial impact is twofold: there is the direct cost of emergency repairs and patching up problems, and the indirect cost of inefficiency—leaky roofs, outdated heating systems, and layouts unsuitable for modern equipment all waste money and hamper staff productivity.
The NHS and Privatisation
There is a lot of talk about privatisation of the NHS. In fact, there are fierce arguments that continually rage around this topic. However, we would rather present the facts to show that the NHS is already being privatised, by the back door and right under our noses!
CLICK HERE to discover how this is being done.
Of course. Here is the new section on clinical negligence and DEI spending, which can be inserted before the conclusion of the blog post.
The Cost of Failure: Clinical Negligence and Administrative Spending
Beyond the debates over funding and privatisation, two other areas represent significant and often controversial financial outflows for the NHS: clinical negligence payouts and spending on Diversity, Equity, and Inclusion (DEI) initiatives.
The Multi-Billion Pound Burden of Clinical Negligence
When medical care goes wrong, the human cost is immeasurable. The financial cost, however, is starkly quantifiable and places an enormous burden on the NHS budget. Clinical negligence occurs when a healthcare professional provides sub-standard care that causes harm to a patient.
The scale of this financial liability is staggering:
- Annual Spend: The NHS Resolution (the health service's claims handling body) pays out over £2 billion annually in damages and legal costs to claimants. In the 2022/23 financial year, the total value of claims paid was £2.6 billion.
- The "Claims Provision": The more telling figure is the total amount set aside for existing and expected claims, known as the "provision". This long-term liability now stands at a colossal £69.4 billion (Source: NHS Resolution, Annual Report and Accounts 2022/23). This is money that must be held in reserve, effectively frozen and unavailable for frontline patient care.
This crisis is driven by several factors, including the rising cost of long-term care for severely injured patients, a legal system that awards damages based on private care costs, and high legal fees. While this system is vital for patients who have suffered genuine harm, it creates a vicious cycle where funds that could be used to improve safety and staffing are instead diverted to pay for past failures.
The Investment in Diversity, Equity, and Inclusion (DEI)
Alongside its clinical and operational costs, the NHS also invests significantly in its workforce and organisational culture through Diversity, Equity, and Inclusion (DEI) programmes. The stated goals are to create a fairer workplace for staff from all backgrounds and to ensure services are equitable for a diverse patient population.
While a full breakdown of "DEI spending" is not centrally published, as it is spread across countless individual trust budgets for dedicated staff, training programmes, and consultancy fees, the scale can be estimated:
- Staff Costs: A 2023 investigation by the Daily Telegraph estimated that NHS trusts in England were spending at least £40 million per year on salaries for dedicated DEI staff.
- Broader Initiatives: This figure does not include the cost of mandatory staff training, external consultants, or the resources spent on producing equality impact assessments and reports. The total opportunity cost—the time clinical staff spend in training sessions instead of with patients—is a further point of debate.
Proponents argue that a more inclusive and equitable NHS is a more effective and efficient one, leading to better staff retention and more targeted patient care. Critics, however, question the return on investment at a time of intense operational and financial pressure, arguing that these millions represent a diversion of funds from frontline clinical priorities.
Conclusion: An Institution at a Crossroads
The financial pressures on the NHS are not simple. While the annual cost of fraud is a shocking £1.14 billion, the systemic issues are far more complex and costly. The crisis in social care, an over-reliance on temporary staff, a potentially bloated management structure, and the real costs of catering to a diverse population all contribute to the strain.
The conversation must move beyond simply "more funding" versus "less funding." It must focus on radical efficiency—fixing the social care system, rationalising the workforce and management, and having an honest, public conversation about the costs and requirements of providing universal healthcare in modern Britain. The goal is to ensure that every possible pound is directed where it belongs: towards effective and efficient patient care.
Sources Cited:
- Institute for Fiscal Studies (IFS). "Health spending." [ifs.org.uk/topics/health-spending]
- NHS Counter Fraud Authority (NHSCFA). "Annual Report and Accounts 2022-23." [cfa.nhs.uk]
- NHS Digital. "NHS Hospital and Community Health Service (HCHS) workforce statistics." [digital.nhs.uk]
- The Health Foundation. "What happened to the NHS workforce during the pandemic?" [health.org.uk]
- Skills for Care. "The state of the adult social care sector and workforce in England." [skillsforcare.org.uk]
- National Audit Office (NAO). "Managing NHS backlogs and waiting times in England." (2022) [nao.org.uk]
- BBC News. "The NHS staff who can't get jobs." (2023) [bbc.co.uk/news]
- Telegraph & Argus. "Bradford midwife role to cut genetic risk in babies." (2014) [thetelegraphandargus.co.uk]
- NHS England. "Latest stats on NHS industrial action." [england.nhs.uk]
- British Medical Association (BMA). "Pay restoration for junior doctors." [bma.org.uk]
- Nuffield Trust. "NHS spending on independent sector providers." [nuffieldtrust.org.uk]
- Department of Health and Social Care. "NHS Estates Returns Collection 2022-23." [gov.uk]
- BBC News. "Musgrove Park Hospital: Roof beam find closes operating theatres." (2023) [bbc.co.uk/news]
- Health Service Journal (HSJ). "The hospitals crumbling from the inside out." (2023) [hsj.co.uk]
- Clinical Negligence: NHS Resolution. (2023). Annual Report and Accounts 2022/23. [Available at: resolution.nhs.uk/resources/annual-report-and-accounts-2022-23/]
- DEI Spending: Donnelly, L. (2023). "NHS spends £40m on diversity managers." The Daily Telegraph. [Available at: telegraph.co.uk/news/2023/07/01/nhs-diversity-managers-cost-40-million/]
If you require assistance with this article, contact us.